Our Research Projects
Overview
“One Health” is a collaborative, multisectoral, and transdisciplinary approach — working at the local, regional, national, and global levels — with the goal of achieving optimal health outcomes recognizing the interconnection between people, animals, plants, and their shared environment” (CDC.gov)
Bacterial infectious diseases are common medical problems in developing countries. Due to limited diagnostic facilities, the causative agents and sources of infection, as well as modes of transmission, often remain unidentified. Empiric treatment is a common practice, fostering the emergence of antibiotic resistance and leading to difficult-to-treat infections. Due to the absence of effective monitoring, knowledge of circulating bacterial strains, their reservoirs and how these change over time, is limited.
Because of our close connection with animals, particularly in developing countries, human infections are often zoonoses. Pathogens can be transmitted to humans through direct contact or through food, water or the environment. Overuse of antibiotics in animal husbandry has significantly contributed to the increase of multidrug resistant bacteria, found both in animals and humans.
Bacteria can also survive for extended periods in the environment. For example, in water, in soil, and of particular concern for human health, in the hospital environment. They are capable of adapting to different environments.
Our research interests cover the generation and comparison of bacteriological data from humans, animals and the environment in countries with limited resources. A special focus is on transmission and the identification of reservoirs of antibiotic resistant bacteria in rural areas of sub-Saharan African countries. Our activities will support and guide patient management and public health measures.
"Antimicrobial resistance in environmental reservoirs and colonizing antibiotic resistant bacteria“-Improving antibiotic use in West Africa: exploring current situation and developing strategies for behavior change
Antibiotic resistance is rising to dangerously high levels in all parts of the world and becoming one of the largest threats to global health and food security. New resistance mechanisms are emerging and spreading globally, threatening our ability to treat common infectious diseases. Antibiotic resistance occurs naturally but is accelerated by poor infection prevention and control and above all by the inappropriate use and overuse of antibiotics. Epidemiological studies have demonstrated a direct relationship between antibiotic consumption and the emergence and dissemination of resistant bacteria. Antibiotic use is not limited to humans but is also widespread in livestock farming as growth promoters, as prophylaxis and to treat infections. The antibiotics used in livestock are ingested by humans when they consume food: molecular detection methods have demonstrated that resistant bacteria in farm animals reach consumers through meat products. The irrational use of antimicrobials is certainly a complex and multifactorial problem in developing countries, and a proper understanding of the problem is necessary for the development of effective control policies. Without behavior change, antibiotic resistance will remain a major threat, even if new medicines are developed.
The overall study is led by project partners from Heidelberg (HIGH) and France (IRD) in collaboration with the BNITM and all partners.
This project aims at understanding and quantify perceptions and uses related to antibiotics among health care workers, communities and livestock farmers and defining patterns of accessing and utilizing antibiotics. Further an intervention to improve awareness and understanding of antimicrobial resistance through effective communication, education and training using a stakeholder-driven approach shall be defined. The focus of our group within this project will be assessing baseline data on AMR pathogens along the food chain in Nouna, Burkina Faso and Kumasi, Ghana.
Partners:
- Kumasi Centre for Collaborative Research in Tropical Medicine (KCCR), Kumasi, Ghana
- Nogouchi memorial Institute for Medical Research (NMIMR), Accra, Ghana
- Council for Scientific and Industrial Research-Animal Research Institute, Accra, Ghana (CSIR-ARI)
- Nouna Health Research Centre (CRSN), Nouna, Burkina Faso
- Institute de Recherche en Sciences de la Santé (IRSS), Ouagadougou, Burkina Faso
- Centre International de Recherche-Devéloppement sur l’Elevage en zone Subhumide (CIRDES),
- Bobo Dioulasso, Burkina Faso
- French National Research Institute for Sustainable Development (IRD)
- Heidelberg University Hospital, Heidelberg Institute of Global health (HIGH)
Funding: Bundesministerium für Bildung und Forschung (BMBF) & French Research National Agency (ANR)
Paediatric Phase I/II study of a vaccine against invasive non-typhoidal salmonellosis in sub-Saharan Africa
Invasive disease with non-typhoidal Salmonella in SSA is associated with increasing antibiotic resistance (AMR) and has been classified by the World Health Organization as high priority for developing new antibiotics. Despite high case fatality rates, particularly in children <5 years of age in SSA countries, no vaccine is currently available. The burden caused by NTS infections and increasing AMR strongly encourage for prompt development of an effective vaccine. A novel vaccine, is currently being developed by GSK Biologicals and GSK Vaccines Institute for Global Health, targeting the serovars Typhimurium and Enteritidis, the most common causative agents of African invasive NTS. Within a large consortium, a paediatric Phase I/II study will be launched early in 2021 in Ghana. The focus of our group will be on antibiotic resistant genotypes of iNTS-causing Salmonella strains. The information gained will not only inform on circulating Salmonella serovars and genotypes but will also inform on the development of AMR pathogens in SSA.
Partners:
Kwame Nkrumah University of Science and Technology (KNUST), Ghana
Kumasi Centre for Collaborative Research in Tropical Medicine (KCCR), Kumasi, Ghana
Agogo Presbyterian Hospital, Agogo, Ghana
University of Siena, Italy
MMGH Consulting GmbH, Switzerland
GSK Vaccine Institute for Global Health (GVGH), Italy
Funding:
European and Developing Countries Clinical Trials Partnership (EDCTP)
Genetic adaptation of Salmonella enterica in human & animal reservoirs in sub-Saharan Africa
Salmonella enterica cause more than 1.2 million annual deaths worldwide, the majority occurring in resource-limited countries. Infections with non-typhoidal Salmonella (NTS) are typically limited to gastrointestinal disease in industrialized countries. In contrast, in sub-Saharan Africa (SSA), NTS are the most frequent cause of bacterial bloodstream infections in adults and children, associated with high fatality rates. In both industrialized countries and SSA, the serovars Typhimurium and Enteritidis cause the majority of infections. In recent years, Salmonella enterica in SSA have also become increasingly resistant to locally available antibiotics, leading to the substantial burden of NTS infections in Africa.
In industrialised countries, infections with NTS are typically of zoonotic origin with regular food-borne outbreaks. In developing countries, studies on transmission reservoirs are limited but previously it has been found that African Salmonella strains have genetically developed by adapting to different hosts or to the environment.
Our research activities focus on transmission including human, animal and environmental reservoirs, antibiotic resistance and genomic characterisation of circulating Salmonella strains in SSA in order to suggest the implementation of effective control strategies.
Partners:
Kumasi Centre for Collaborative Research in Tropical Medicine (KCCR), Kumasi, Ghana
Agogo Presbyterian Hospital, Agogo, Ghana
National Institute for Medical Research (NIMR) in Tanga, Tanzania
Korogwe District hospital, Korogwe, Tanzania
Funding: German Research Foundation (DFG)

Antibiotic resistant enteric pathogens in human and animal reservoirs
In resource-limited countries, broad-spectrum antibiotics are often prescribed empirically without microbiological diagnosis. This overuse of antibiotics in human medicine, significantly contributes to the emergence and the increase of multidrug-resistance. In addition, the use of antibiotics in animal husbandry as growth promoters and for prophylaxis and treatment of infection aggravates this problem. Often, in countries where resources are limited, animal farming is a common occupancy and people often live in close proximity to animals. Animals and meat products have been suggested as an important source for drug resistant enteric pathogens including Campylobacter spp., Arcobacter spp., Salmonella enterica, ESBL-producing Escherichia coli and Klebsiella pneumoniae in SSA countries. Transmission of these bacteria might occur by direct contact or consumption of contaminated meat products, leading to the colonization of the intestinal tract and eventually to infections. So far, the degree to which animals play a role as a reservoir for the transmission of multi drug resistant bacteria has not been studied on genotype level in rural areas of SSA. Within this project, Campylobacter spp., Arcobacter spp., Salmonella enterica, ESBL-producing E. coli and K. pneumoniae genomes collected from human and animals will be compared to examine transmission between human and animal in rural areas of Tanzania and Ghana.
Partners:
Kumasi Centre for Collaborative Research in Tropical Medicine (KCCR), Kumasi, Ghana
Agogo Presbyterian Hospital, Agogo, Ghana
National Institute for Medical Research (NIMR) in Tanga, Tanzania
Korogwe District hospital, Korogwe, Tanzania
Funding:
German Research Foundation (DFG)

Bacterial subtypes and their association with diarrhoea
Globally, one in ten child deaths during the first five years of life result from diarrhoeal disease. Due to limitations in diagnostic facilities in resource-constrained clinical settings, the aetiological agent of diarrhoeal disease is rarely laboratory confirmed. In the past years, clinical studies on diarrheal diseases in developing countries have shed more light on the predominating causes of infection. Campylobacter spp., Shigella spp., and diarrhoeagenic Escherichia coli and Salmonella enterica have been among the most common pathogens isolated from patients with diarrhoea. So far, studies on Arcobacter spp. are limited. Arcobacter spp. is an emerging pathogen with its role in diarrhoeal disease not well understood. In the past years, moderate associations with diarrhoea have been demonstrated for Shigella spp., Campylobacter spp. and diarrhoeagenic Escherichia coli but the associations on bacterial sub-type level have not been studied thoroughly. Data on sub-type specific burden of diarrhoea and antibiotic resistance is needed in order to identify populations at risk, to develop preventive measures and to adjust antibiotic usage when treatment is indicated.
Within this study we investigate and compare bacterial subtypes of children below 5 years of age and the association with diarrhoea in a rural hospital in Tanzania.
Partners:
National Institute for Medical Research (NIMR) in Tanga, Tanzania
Korogwe District hospital, Korogwe, Tanzania
Funding:
German Center for Infection Research (DZIF)
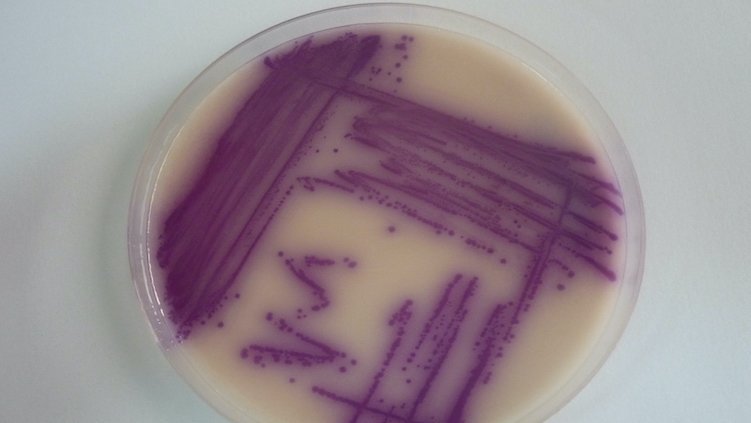
Antimicrobial resistance surveillance in sub-Saharan Africa
The spread of antimicrobial resistance (AMR) is a major challenge for health systems worldwide, also affecting many African countries. The majority of bacterial infections with resistant pathogens in sub-Saharan Africa still go undetected and empiric treatment of infections is common. The reason behind are lack of microbiology laboratories, that are capable of performing bacterial culture and antibiotic susceptibility testing, particularly in rural areas of sub-Saharan Africa. Therefore, the GHP funded project “development of standardized AMR laboratories” has so far built and set up three fully functioning AMR microbiology laboratories in three different geographical locations of Ghana, namely Agogo (Asante Akim North District), Assin Fosu (Assin Fosu Municipal) and Agroyesum (Amansie West District). The established laboratories are standardized and are able to process clinical specimens such as blood, urine and stool samples as well as perform antibiotic susceptibility testing according to the guidelines of the WHO Global Antimicrobial Resistance Surveillance System (GLASS). The established AMR surveillance systems will inform on circulation and emerging AMR bacterial strains and will eventually lead to improved patient care by allowing targeted antibiotic treatment. Currently, this work is expanded to three study sites in Tanzania including the island of Zanzibar. Work is carried out in collaboration with the National Institute for Medical Research (NIMR), the Zanzibar Livestock Research Institute (ZALRI) and the Health Improvement Project Zanibar (HIPZ).
Partners:
National Institute for Medical Research (NIMR), Tanga, Tanzania
Bombo Regional Referral Hospital, Tanga, Tanzania
Korogwe District Hospital, Korogwe, Tanzania
Health Improvement Project, Zanzibar, Tanzania
Makunduchi Health Centre, Zanzibar, Tanzania
Kumasi Centre for Collaborative Research in Tropical Medicine (KCCR), Kumasi, Ghana
Agogo Presbyterian Hospital, Agogo, Ghana
St. Francis Xavier Hospital, Assin Fosu, Ghana
St. Martin Catholic Hospital, Agroyesum, Ghana
Funding: Global Health Programme (GHP)-Bundesministerium für Gesundheit
Transmission reservoirs and acquisition of multidrug resistant bacteria in neonates admitted to two hospitals within the Tanga Region of Tanzania
Infections with antibiotic resistant bacteria are common medical problems in developing countries leading to significant morbidity and mortality in particular affecting vulnerable groups such as children under the age of five and neonates. Due to limited diagnostic facilities in countries with low resources, the causative agents and sources of infection, as well as modes of transmission, often remain unidentified. Due to the absence of effective monitoring and surveillance systems, knowledge of circulating bacterial strains, their reservoirs and how these change over time, is limited, however this is essential information for successful patient management and for the implementation of control strategies.
The WHO has developed a pathogen priority list divided into three categories according to the urgency of need for new antibiotics: critical, high and medium priority. The most critical group includes multi drug resistant bacteria that pose a particular threat in hospitals. They include Acinetobacter baumannii (carbapenem resistant) Pseudomonas aeruginosa (carbapenem resistant) and bacteria of the group Enterobacterales, including Klebsiella spp. and Escherichia coli (carbapenem resistant and ESBL-producing).
This study aims at generating data in the field of multidrug resistant bacteria (WHO prority pathogen), their reservoirs in community and hospital environments with a focus on maternal-neonatal transmission in order to improve hospital hygiene and prevention programs.
Partners:
National Institute for Medical Research (NIMR), Tanga, Tanzania
Bombo Regional Referral Hospital, Tanga, Tanzania
Korogwe District Hospital, Korogwe, Tanzania
Funding: Global Health Programme (GHP)-Bundesministerium für Gesundheit
Capacity Building Projects
Hospital partnership, Tanzania
In many African countries, in particular those of sub-Saharan Africa, fever is still mainly associated with malaria. Fortunately, malaria diagnostics such as microscopy and rapid test are largely available, even in resource limited clinical settings. This is less true for differential diagnosis of other febrile illnesses such as for example those caused by bacteria that are potentially severe and for which specific treatment is required. Most hospitals in Tanzania do not offer such differential diagnosis and antibiotic susceptibility testing is not routinely carried out. As a result, empiric treatment is typically applied. This leads to overuse of antibiotics and to treatment failures.
Partners:
National Institute for Medical Research (NIMR), Tanga, Tanzania
Bombo Regional Referral Hospital, Tanga, Tanzania
Funder: Deutsche Gesellschaft für Internationale Zusammenarbeit (GIZ)
Within this project we aim at improving clinical and laboratory capacities in the field of differential diagnosis of febrile illnesses, other than malaria with a focus on bacteremia/sepsis. In addition, clinical and laboratory personnel will be trained in the field of gastrointestinal and urinary tract infections. We also offer training support in antibiotic stewardship and clinical algorithms.
This project will not only support ongoing research activities but in the long term will contribute to generate data on circulating antibiotic resistant bacteria within the Tanga region and will allow the hospital to produce its own annual report on nosocomial and community acquired antibiotic resistant bacteria.
Partners:
National Institute for Medical Research (NIMR), Tanga Tanzania
Bombo Regional Referral Hospital, Tanga, Tanzania
Korogwe District Hospital, Korogwe, Tanzania

Antimicrobial resistance in sub-Saharan Africa - Improving Diagnostics and Understanding Risk Factors - A project of the COMBAT AMR in Africa Network
The overuse of antibiotics in healthcare and livestock farming has led to a global rise in antibiotic resistance, with the most severe consequences seen in low and middle-income countries (LMICs). In LMICs, crucial antibiotics for treating antimicrobial resistance (AMR)-related infections are often scarce and expensive, disproportionately affecting low-income populations. Additionally, antibiotic susceptibility testing (AST) is often unavailable or costly, preventing proper identification of patients who could benefit from AST-guided antibiotic treatment.Without intervention, an estimated 10 million people worldwide may die annually from infections caused by multi-drug resistant (MDR) pathogens by 2050. To address this crisis, the World Health Organization (WHO) has launched a Global action plan on antimicrobial resistance.
A One Health approach, recognizing the interconnectedness of human, animal, and environmental health, is crucial in combating AMR. However, many countries lack detailed data on colonization rates in different populations, such as healthcare workers (HCWs), potential vectors like houseflies, and the role of links between humans and animals, such as slaughter cattle and slaughterhouse employees.
To address these issues, we established the COMBAT AMR in Africa network and propose a multicenter study at 8 partner sites in sub-Saharan Africa. This project aims to improve diagnostics for infectious diseases caused by multidrug-resistant Gram-negative bacteria and understand MRGN colonization risk factors.
In Work Package 1, we will assess MRGN colonization rates in cattle and humans, including HCWs and slaughterhouse employees, comparing them to control groups. In Work Package 2, we will evaluate the clinical value of rapid AMR protein testing, aiming to expedite the diagnosis of MDR infections and enable early targeted antibiotic treatment. This project, centered at Asella Teaching and Referral Hospital in Ethiopia, addresses critical AMR challenges in LMICs within a One Health framework.
Microbiome and resistome of Mycobacterium ulcerans lesions
Buruli ulcer is one of the infectious diseases that has been recognised as “neglected tropical disease” by the World Health Organization (WHO, 2015). It is caused by the bacterial pathogen Mycobacterium ulcerans and occurs primarily in poor urban and in rural settings of developing countries such as sub-Saharan Africa. Within this project we aim at determining antimicrobial resistance in M. ulcerans isolated from Buruli ulcer lesions in rural Ghana. Further, the microbiome flora of unaffected and affected skin will be analysesd to determine the impact of the microbiome on delayed wound healing.
The lead of this project is taken by the Department Infectious Disease Epidemiology (Dr Thorsten Thye, thye@bnitm.de). Our group will analyse secondary infections with antibiotic resistant bacteria within this work.
Partners:
Kumasi Centre for Collaborative Research in Tropical Medicine (KCCR), Kumasi, Ghana
Funding:
German Research Foundation (DFG)