FAQ on the Marburg virus
Disclaimer
The contents of this website are for general information purposes only and do not constitute medical advice, diagnosis or treatment. They are not a substitute for individual consultation with a qualified medical professional.
No guarantee is given for the accuracy, completeness or timeliness of the information provided. Use of the content is at your own risk. If you have any health questions or complaints, please always consult a doctor or other qualified professional.
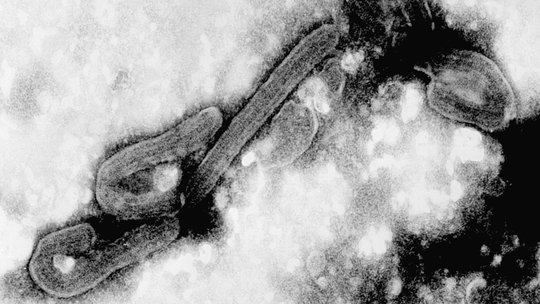
1. What are Marburg viruses and where do they occur?
Marburg virus disease (MVD) is caused by the Marburg virus which is, like the Ebola virus, an animal-borne RNA virus of the filovirus family. Until now, Marburg virus disease was known to occur in eastern, central and southern Africa. In 2021, scientists identified a patient with this disease in West Africa for the first time.
2. What are the symptoms of infection?
The Marburg virus can cause haemorrhagic fever in infected persons, which is fatal in 24 to 88 percent of cases depending on virus strain and case management (WHO). As the World Health Organization (WHO) states on its website (www.who.int/news-room/fact-sheets/detail/marburg-virus-disease), after an incubation period of two to 21 days, symptoms such as high fever, strong headache and myalgia may appear. Vomiting, chest pain, sore throat, abdominal pain and severe watery diarrhoea may also occur. Symptoms become increasingly severe and may include massive bleeding and multi-organ failure.
3. How are Marburg viruses transmitted?
One of the reservoirs for the Marburg virus is the African fruit bat Rousettus aegyptiacus. Close contact with Marburg virus patients or with their body fluids like blood can lead to infection.
4. Which treatment do we know?
So far, there is neither a specific treatment for Marburg virus disease nor a vaccine. However, supportive care like rehydration with oral or intravenous fluids and treatment of specific symptoms improves survival.
5. More information?
- The following website of the WHO provides further and detailed information: www.who.int/news-room/fact-sheets/detail/marburg-virus-disease
- Our recent publication in the New England Journal of Medicine (NEJM) highlights the importance of effective outbreak management, 30.6.2022: Press release BNITM 30.6.22.
- BNITM news from 8.12.2017: Europäisches Mobiles Labor bei Marburg-Virus-Ausbruch in Uganda
Contact
- Prof. Dr Stephan Günther
- Head of Virology Department
- phone: +49 40 285380-547
- fax: +49 40 285380-459
- email: guenther@bnitm.de
- Prof. Dr César Muñoz-Fontela
- Research Group Leader
- phone: +49 40 285380-548
- fax: +49 40 285380-512
- email: munoz-fontela@bnitm.de
- Dr Anna Hein
- Public Relations
- phone: +49 40 285380-269
- email: presse@bnitm.de
- Julia Rauner
- Public Relations
- phone: +49 40 285380-264
- email: presse@bnitm.de
- The Laboratory diagnostics|Consultation for physicians
- Advice on the diagnostic procedure
- phone: +49 40 285380-211
- fax: +49 40 285380-252
- email: labordiagnostik@bnitm.de