Global threat from antibiotic resistance
Study: Number of annual deaths almost doubled since 1990
Antimicrobial resistance (AMR) is one of the greatest global health threats of our time. In a comprehensive study, an international research network, including researchers from the Bernhard Nocht Institute for Tropical Medicine (BNITM), has analysed the global development of bacterial resistance between 1990 and 2021 for the first time and drawn up forecasts up to 2050 - with alarming results: without sturdy countermeasures, the annual deaths caused by resistant bacteria could almost double by 2050. The study conducted by the international research consortium Global Burden of Disease (GBD) has been published in the scientific journal Lancet.
Antimicrobial resistance (AMR) occurs when bacteria become resistant to antibiotics. This makes it considerably more difficult to treat bacterial infections such as pneumonia, sepsis, urinary tract or skin infections. Among the most severely affected bacteria are Escherichia coli, which often causes urinary tract infections, Staphylococcus aureus, which can cause skin and lung infections that are difficult to cure, and Klebsiella pneumoniae, which causes dangerous respiratory infections, particularly in immunocompromised individuals. If such bacteria become resistant to antibiotics, infections can no longer be treated effectively. The consequences are more severe disease, higher mortality rates and rising costs for the healthcare system.
The Global Burden of Disease (GBD) Antimicrobial Resistance Collaborators are studying how antimicrobial resistance is developing over time. Their latest meta-analysis, ‘Global burden of bacterial antimicrobial resistance 1990–2021: a systematic analysis with forecasts to 2050’, is the first global survey of deaths directly or indirectly attributable to antimicrobial resistance. In an earlier study, the GBD quantified the global and regional burden of AMR for 2019, followed by further publications that provided more detailed estimates for several WHO regions by country. Until now, there have been no studies that provide comprehensive estimates of the burden of AMR in different locations, taking into account historical trends and future projections.
The research team evaluated data from 204 countries and regions on 22 pathogens, 84 pathogen-drug combinations, and 11 infectious syndromes. The analysis was based on over 520 million data sets, including microbiological data, hospital discharge data, mortality registers, pharmaceutical sales figures, and surveys on antibiotic use. The Kumasi Centre for Collaborative Research in Tropical Medicine (KCCR) in Ghana, co-operated by the BNITM, also contributed important scientific data.
Using statistical modelling, the researchers then produced global and regional estimates of the burden of AMR between 1990 and 2021. To better understand the impact of AMR, they simulated two scenarios. In the first scenario, they calculated how many annual deaths and cases of disease there would have been if all infections with resistant bacteria had still responded to antibiotics. In the second scenario, they assumed that there were no infections at all. These approaches helped to calculate the actual burden of resistant bacteria. In addition, the team made projections up to 2050. They modelled how deaths due to AMR might develop – for example, if healthcare were to be improved worldwide or new antibiotics developed.
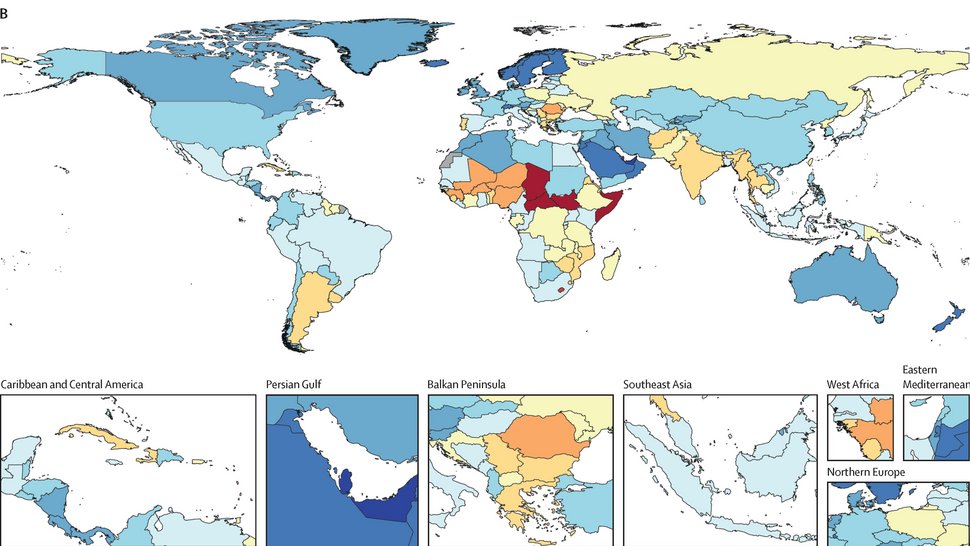
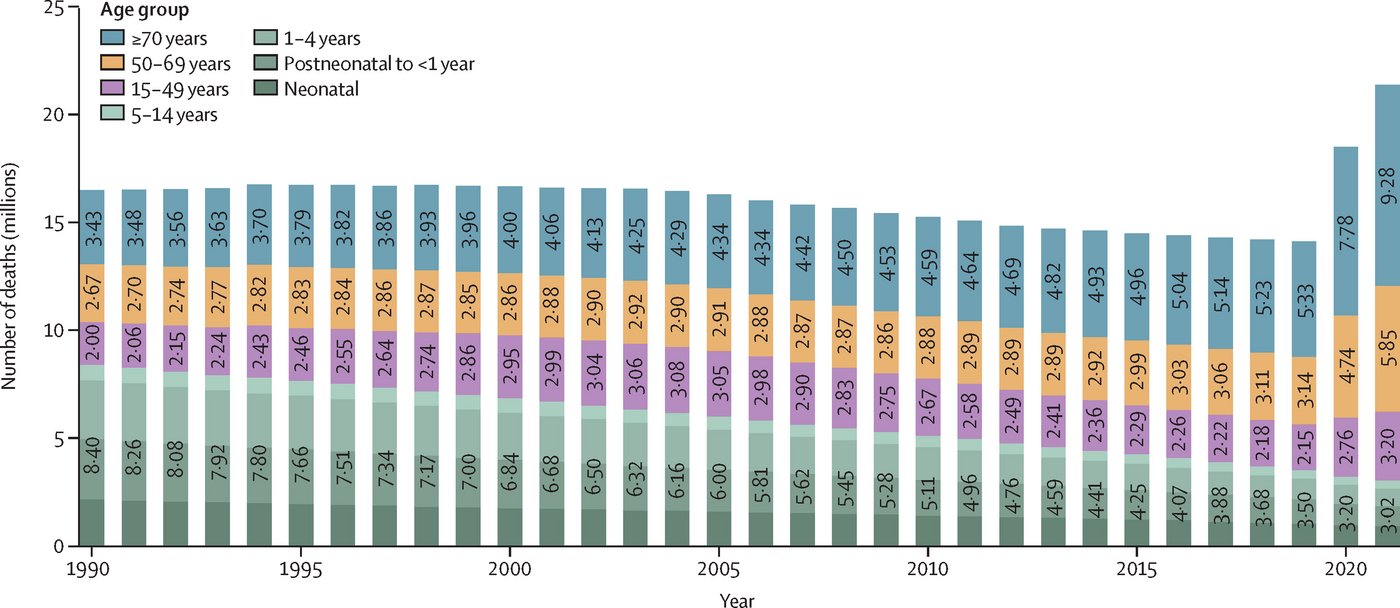
Large differences by age and region
The results are alarming: the researchers estimate that between 4 and 7.1 million deaths worldwide in 2021 were associated with bacterial AMR, 1.14 million of which were directly attributable to it. There are major differences depending on age and region: while deaths among children under the age of five have fallen by over 50 per cent since 1990, they have increased by more than 80 per cent among people aged 70 and over. These opposing trends reflect medical progress in the treatment of children, but at the same time emphasise the growing threat to older people, whose immune systems are more vulnerable due to age and previous illnesses.
In terms of individual bacterial strains, methicillin-resistant Staphylococcus aureus (MRSA) showed the strongest increase: associated deaths rose from 261,000 in 1990 to 550,000 in 2021, and deaths directly attributable to it from 57,200 to 130,000. Among Gram-negative bacteria, resistance to emergency antibiotics from the carbapenems group in particular increased, with an increase in associated deaths from 619,000 to over one million in 2021.
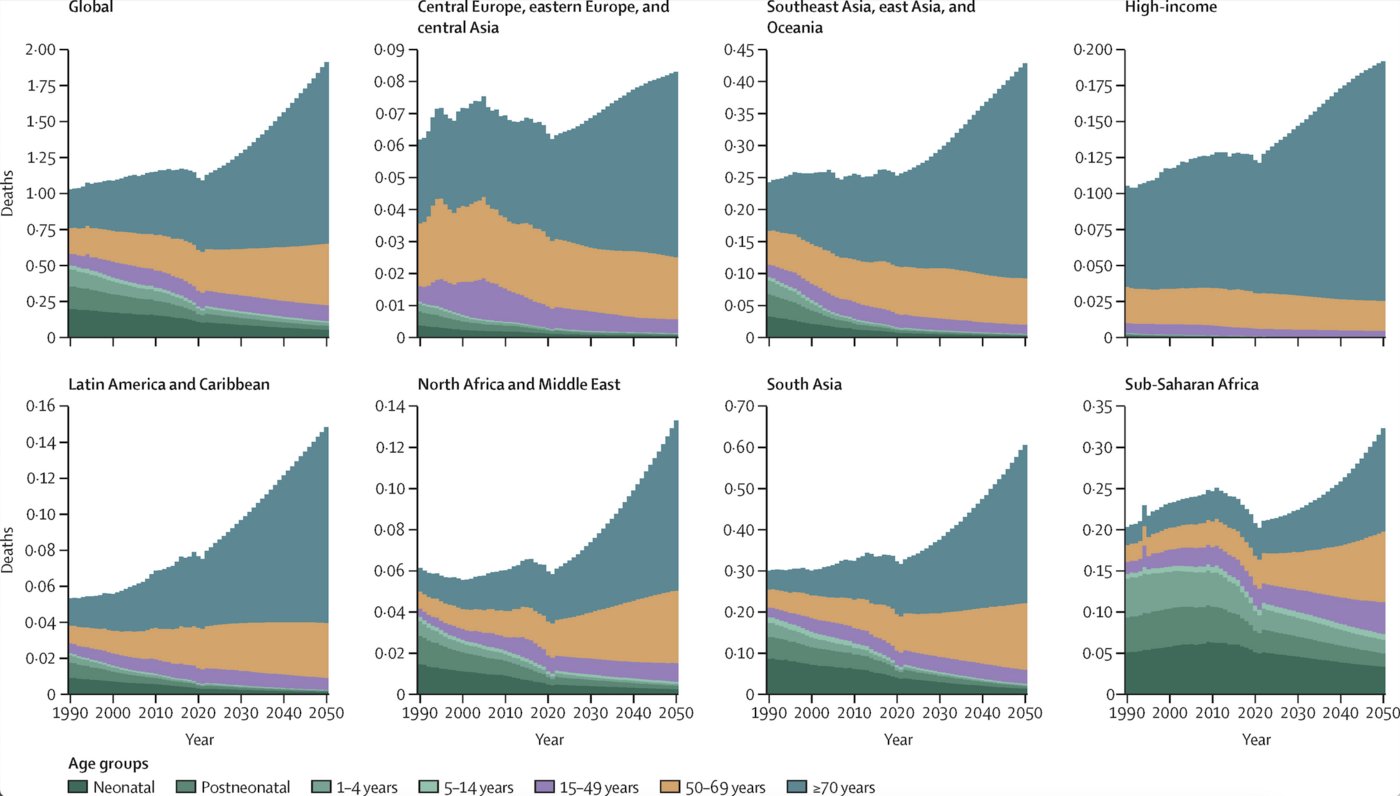
Forecasts for 2050 suggest that almost 2 million deaths worldwide could be directly attributable to AMR by then, and up to 8.22 million indirectly. Southeast Asia and Latin America are expected to be particularly affected.
Despite the alarming figures, there are also positive signs: the study shows that up to 92 million deaths could be avoided between 2025 and 2050 through improved healthcare and the more targeted use of antibiotics. The development of new antibiotics, particularly to combat Gram-negative pathogens, could save an additional 11 million lives.

“This study is a wake-up call for the international community. The development of new drugs and the targeted use of antibiotics are essential to overcome the looming AMR crisis,” says Prof. Jürgen May, BNITM Chairman and Head of the Department of Infection Epidemiology, which played a major role in the study.
“We need to use fewer antibiotics, both in medicine and in cattle, and when we do, we need to use them in a targeted manner, depending on the pathogen and the infection. We also need to strengthen surveillance systems, advance the development of new drugs and improve access to vaccinations and clean water,” adds co-author Dr Denise Dekker, head of the One Health Bacteriology working group at the BNITM. “Our goal must be to prevent infections before they occur,” she says.

The comprehensive analysis of the global AMR burden provides decision-makers with valuable insights to develop targeted measures against the spread of resistant bacteria. Particularly in countries with limited access to adequate healthcare, investing in public health and developing new treatment approaches is urgently needed to save millions of lives.
Original publication
Global burden of bacterial antimicrobial resistance 1990–2021: a systematic analysis with forecasts to 2050. The Lancet, Volume 404, Issue 10459, 28 September–4 October 2024, Pages 1199-1226.
Background
The Global Burden Disease Consortium (GBD) is an international network of researchers. Its goal is to quantify the global burden of disease. To do this, it collects and analyses data from over 200 countries and territories, and uses this data to produce comprehensive estimates of the frequency and severity of diseases, injuries and risk factors worldwide. More than 9,000 scientists from 162 countries work together to paint a detailed picture of the global health situation. The results provide decision-makers and health authorities with valuable insights for developing targeted prevention strategies and measures to improve the health of the world's population.
Contact person
Prof. Dr Jürgen May
Head of Dpt. Infectious Diseases Epidemiology
Phone : +49 40 285380-402
Email : may@bnitm.de
Julia Rauner
Public Relations
Phone : +49 40 285380-264
Email : presse@bnitm.de
Further information