First scientific study on snakebites in Malawi provides important epidemiological data
When it comes to snakebites, three things count: speed, well-trained medical staff and an effective antivenom. The first study on snakebite poisoning in Malawi, "Health care workers' knowledge on identification, management, and treatment of snakebite cases in rural Malawi", shows that there is still room for improvement. It was recently published in the journal PLOS Neglected Tropical Diseases.

Snakebite envenoming is one of the poverty-associated neglected tropical diseases (NTDs). The World Health Organisation (WHO) estimates that snakes bite about 5.4 million people every year, poisoning 2.7 million. Up to 140,000 of the victims die, about three times as many are injured. Sub-Saharan Africa, South and South-East Asia and Latin America are affected most.
Snakebite envenoming is also a significant health problem in the south-east African state of Malawi. However, there is little data available, neither on the actual number of cases, nor on the medical treatment of snakebite victims, nor on whether they use medical facilities at all. There is little literature on what medical personnel know about snakes, how they deal with snakebite envenoming and what antivenoms are available to them.
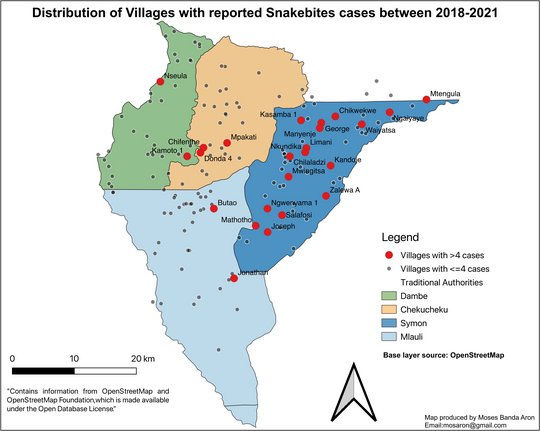
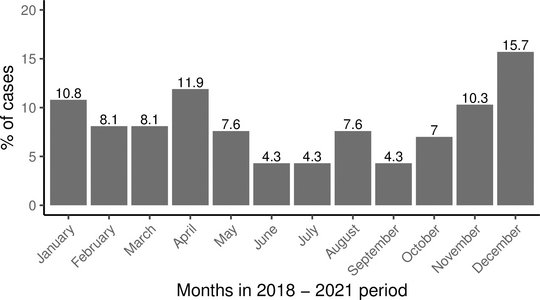
An international cross-institutional research group has now conducted the first scientific study on the epidemiology of snakebite envenoming in Malawi. Moses Aron, a Malawian PhD student in the Snakebite Envenoming Research Group of Dr Jörg Blessmann and Dr Benno Kreuels within the newly established Department of Implementation Research at the Bernhard Nocht Institute for Tropical Medicine (BNITM), conducted this study with other researchers from Malawi and Germany. He wanted to find out whether health care workers can recognise the snake species found in Malawi, how they assess their venomousness and how they treat snakebite victims medically. To do this, he interviewed medical and nursing staff at the 15 health facilities in Neno district in the southwest of the country and studied patient registers from 2018 to 2021. In the records, he found 185 registered snakebite cases. This represents an annual average of 36 cases per 100,000 population - the first snakebite incidence ever reported for a district in Malawi.
Discrepancy between risk assessment and knowledge
105 doctors, pharmacists, medical technicians and nurses were interviewed. Almost 90 per cent reported snakebite envenoming as a problem in the district. Many reported examples from their professional practice and complications up to amputations.
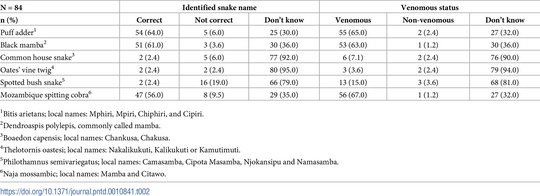
While two-thirds of respondents recognised venomous snakes, 90 per cent could not correctly identify nonvenomous snakes. Ninety-five percent reported that snakebite victims were more likely to go to traditional healers than to hospital. The reasons they gave were: too far from the hospital, too high cost, lack of antivenom, mistrust, ignorance and superstition. This suggests that the actual number of snakebite poisonings in Malawi is much higher than the hospital registers indicate.
A good 70 per cent of health workers asserted that they had been trained in the treatment of snakebite victims, but most of them not as part of continuing professional development. Guidelines for the treatment or management of snakebites in health facilities were largely unavailable.
Available antidotes: Not available
The choice, dosage and administration of antidotes sometimes seem to vary widely. Most study participants did not know the composition of antivenoms and rated the correct administration of the drug as difficult.
An antivenom effective against several snake venoms was only available in two hospitals at the time of the survey. However, there is not yet sufficient clinical data on whether it is also effective against snake venoms found in Malawi. Other clinically tested products available on the African market are effective against the venom of the West African sand rattle viper, but this does not occur in Malawi. Other available preparations either lack data or have proven to be ineffective.
"This first study has confirmed the expectations of us Malawian colleagues that treatment guidelines, regular training and effective antidotes are needed in Malawi," says first author Moses Banda Aron. This retrospective study is just a beginning. "The next step now is a systematic prospective collection of data on snakebite patients." Aron assumes that with further training, treatment could be improved and with a clinical database, the (in)effectiveness of the existing preparation could be proven.
Victims of snakebites have been shown to change their health behaviour when their community is sensitised to the issue and antivenoms are available. WHO also recommends that health care workers work with traditional healers.
More studies are needed in Neno to understand health service seeking behaviour, local beliefs and knowledge about snakebites in communities. In addition, more epidemiological studies are also needed to understand the full extent of the snakebite envenoming problem. The latter would also help to assess the need for antivenom and could facilitate its procurement and provision.
Original publication:
Aron, Moses Banda et al.: Health care workers’ knowledge on identification, management and treatment of snakebite cases in rural Malawi: A descriptive study. Plos Neglected Tropical Diseases Nov 21, 2022.
Contact person
Dr Jörg Blessmann
Research Group Leader
Phone : +49 40 285380-722
Email : blessmann@bnitm.de
Dr Benno Kreuels
Research Group Leader
Phone : +49 40 285380-723
Email : kreuels@bnitm.de
Dr Eleonora Schoenherr
Public Relations
Phone : +49 40 285380-269
Email : presse@bnitm.de
Julia Rauner
Public Relations
Phone : +49 40 285380-264
Email : presse@bnitm.de
Further information